Acting like a hinge, the knee is the largest joint in human body. It supports weight and responds to many forms of leg movement, and so it is persistently subjected to tremendous pressure and easily injured. Knee pain and injuries may emerge from various traumas incurred during exercise or everyday activities, like running or squatting.1 These injuries often involve multiple structures, such as tearing of soft tissues (e.g. ligaments, meniscus and tendons), bone fractures, or dislocations (e.g. kneecaps or cartilage), which can make the situation more complicated.2
The anterior cruciate ligament (ACL) tear is the most common type of serious knee injury in sports, with about 3,600 new cases in Hong Kong yearly.3 Strenuous sports with vigorous body contact aren’t the only activities that put your knee at risk; non-contact injuries also occur. In fact, approximately 70% of ACL tears involve minimal or no contact.4 Any type of activity that imposes stress on the knee, or involving sudden stops or turns, can be injurious. The risk of an ACL injury lies hidden in everyday life, because these injuries occur during regular, everyday activities, not just sports. It must not be taken lightly. 5

What is this article about?
- Did I tear my ACL?
- What is the Anterior Cruciate Ligament (ACL)?
- What are the possible causes of ACL injuries?
- What are the signs and symptoms of an ACL injury?
- Am I at high risk for ACL Injuries?
- How is an ACL Injury diagnosed?
- What should I do if I have injured my ACL?
- How can I prevent an ACL injury?
Did I tear my ACL?
Knee pain and swelling are two typical symptoms of knee injuries and disorders. You may also feel unstable or as if your knee is buckling. The following four questions can help you to identify an ACL injury.
Question 1 — What is the Anterior Cruciate Ligament (ACL)? 5-9
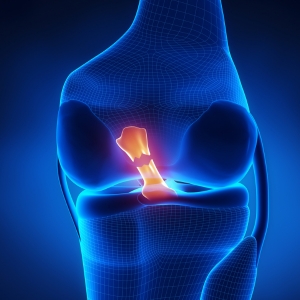
Moving your leg seems so simple, but every single gesture involves precise movements and complex coordination of joint components. In the knee joint, where the thigh bone and shin bone join at the kneecap, there are four elastic band-like ligaments connecting the bones together. One of these, the ACL, helps to stabilize the joint by limiting excessive movement during flexion, extension or rotation. It provides major resistance to stop forward sliding and contributes to the rotational stability of the knee at full extension.
Question 2 — What are the possible causes of ACL injuries? 6,9-10
The ACL is the ligament most at risk of tearing or sprains, as it bears incredible tension exerted in a number of directions, especially in back-and-forth movement.
Any motion that involves abruptly turning or stopping—for example, a sudden change in direction during deceleration, falling, or landing from a jump—can be injurious to the ACL.
Question 3 — What are the signs and symptoms of an ACL injury? 6,7
Typically, you may hear a “pop” at the instant an injury occurs, indicating that the ligament has broken. Due to bleeding or tissue damage, patients with a torn ACL are prone to develop swelling, which may result in stiff and painful knees. You may also feel weakness and instability in your leg, with a buckling that leaves you unable to bear weight. Knee pain or instability may occur when you try to stand up.
In some cases, patients may experience only slight swelling, and minimal or even no pain. You might still feel good to continue your activities. However, symptoms sometimes take a few hours to develop, so don’t ignore any mild signs. Stay vigilant about your condition.
Question 4 — Am I at high risk for ACL Injuries? 11,12
An ACL tear can happen at any age, but certain factors may indicate a higher chance of suffering an ACL injury:
- People who engage in physical work or sports that involve sudden changes of direction have a higher risk of an ACL tear.
- A prior history of ACL injuries is a serious risk factor. Patients with a prior ACL injury within the past 12 months were 11 times more likely to injure their graft or contralateral ACL than those who were previously uninjured.
- Females are at higher risk than males.
- Other extrinsic risk factors include improper footwear or sport gear, and environmental factors such as weather and ground conditions. These may put a person off-balance easily and increase the risk of injury.
- Heavy weight and improper movement patterns or gestures may also lead to a higher chance of ACL injuries.

How is an ACL Injury diagnosed? 13
Usually, a diagnosis is made based on physical examination. Besides checking for swelling and tenderness, your doctor may move your leg in varying positions to assess the range of motion and the overall function of the joint. X-rays often follow, to rule out bone fractures or dislocations. An MRI scan is indicated to confirm the diagnosis and to determine whether there has been damage to other hard and soft tissues such as the meniscus, articular cartilage, and collateral ligaments.
What should I do if I have injured my ACL?
Patients with ACL injuries should receive an early diagnosis and appropriate rehabilitation, or reconstructive surgery if necessary.
Acute Management5
If you have injured your knee, proper first-aid treatment to relieve pain and ease swelling can make you feel much better. The R.I.C.E. method is a simple self-care technique:
Rest: Stop and rest to avoid adding stress to the injured area.
Ice: Apply an ice bag to reduce pain and swelling.
Compression: Wrap the injured area with a bandage or compression wrap to prevent swelling.
Elevation: Lie down and elevate the injured knee.
Nonsurgical Treatment and Surgical treatment14,15
Your choice of treatment should include detailed considerations of multiple factors such as your age, sports you participate in or your activity level, the severity of the injury, and the extent of the instability.
Nonsurgical treatment is usually recommended for older patients or those with less active lifestyles. It focuses on intensive rehabilitation aimed at preventing deficits in knee extension, restoring strength, and preserving stability. Patients should practice a set of specific exercises that counteract anterior shin bone translation to restore their knee function and strengthen the muscles.
If the knee is severely injured to the extent that rehabilitation alone will offer no improvement, or for patients that engage in physically demanding sports, surgery is recommended to fully restore leg function. In ACL reconstruction treatment, the damaged ligament tissue will be replaced with a piece of tendon from another part of your knee. Anti-inflammatory drugs are prescribed to reduce pain and swelling when necessary. A knee brace can be helpful to prevent a patient’s knee from moving and hold the bones in place during recovery.
How can I prevent an ACL Injury?
Though ACL injuries are serious and debilitating, there are some simple measures you can take to minimize the risk of ACL tears.
Firstly, strengthen your muscles. When the muscles surrounding the knees grow strong and flexible, the ACL is more resilient against trauma. Secondly, improve your balance and coordination to reduce the risk of unnatural twists or being put off-balance, and practice proper techniques and postures to avoid the sorts of motions that can cause injuries. Fatigue affects your physical performance, so avoid exercising when you are tired. You should also be sure to wear proper footwear or sports gear.11
Remember to warm up every time you exercise, as cold and stiff muscles are prone to injury. The FIFA 11+ injury prevention programme is a set of exercises designed by FIFA and proven to significantly reduce injuries and enhance performance. It includes a practical and helpful approach to warm-up exercises.16,17
If you want to receive more specific medical advice, contact the Matilda Orthopaedic and Spine Centre at 5501 6699 or This email address is being protected from spambots. You need JavaScript enabled to view it. to arrange an appointment with our specialist.
The above information is provided by Dr. Kong Chi Chung.
Articles on this website are informative only and not intended to be a substitute for professional medical advice, diagnosis or treatment. They should not be relied upon for specific medical advice.
Reference:
1. Nessler T, Denney L, Sampley J et al. Curr Rev Musculoskelet Med. 2017;10:281-288.
2. OrthoInfo. Common Knee Injuries Available from: https://orthoinfo.aaos.org/en/diseases--conditions/common-knee-injuries/ [Accessed 27 Oct 2022].
3. Hospblog. 推廣運動醫學要「貼地」熱血團隊致力社區實踐. Available from: https://www3.ha.org.hk/ntec/dr_hospblog/hospblog.asp?id=177 [Accessed 27 Oct 2022].
4. Pfeifer CE, Beattie PF, Sacko RS,. Int J Sports Phys Ther. 2018;13:575-587.
5. Evans J, Nielson JL. Anterior Cruciate Ligament Knee Injuries. 2022 May 5. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–.
6. Cleveland Clinic. ACL (Anterior Cruciate Ligament) Tears. Available from: https://my.clevelandclinic.org/health/diseases/16576-acl-anterior-cruciate-ligament-tears [Accessed 27 Oct 2022].
7. University of Michigan Health. Anterior Cruciate Ligament (ACL) Injuries. Available from: https://www.uofmhealth.org/conditions-treatments/cmc/knee/acl [Accessed 27 Oct 2022].
8. O'Connor. J, Avatsky, A. Biomecánica. 1995;3:121-132.
9. Escamilla RF, Macleod TD, Wilk KE. J Orthop Sports Phys Ther. 2012;42:208-20.
10. Raines BT, Naclerio E, Sherman SL. Indian J Orthop. 2017;51:563-575.
11. Bradsell H, Frank RM. T. Ann Joint. 2021;7.
12. Jagadeesh N, Kapadi S, Deva V, et al. Risk Factors of ACL Injury. In: Suarez-Ahedo, C. , editor. Arthroscopy [Internet]. London: IntechOpen; 2021 [Accessed 2022 Oct 28].
13. Musahl V, Citak M, O'Loughlin PF, et al. Am J Sports Med. 2010;38:1591-7.
14. Bogunovic L, Matava MJ. Operative and nonoperative treatment options for ACL tears in the adult patient: a conceptual review. Phys Sportsmed. 2013;41:33-40.
15. OrthoInfo. ACL Injury: Does It Require Surgery? Available from: https://orthoinfo.aaos.org/en/treatment/acl-injury-does-it-require-surgery/ [Accessed 27 Oct 2022].
16. Sigurðsson HB, Briem K, Grävare Silbernagel K. Int J Sports Phys Ther. 2022;17:823-831.
17. Sadigursky D, Braid JA, De Lira DNL, et al. BMC Sports Sci Med Rehabil. 2017;9:18.

Information provided by:
DR. KONG Chi Chung, Specialist in Orthopaedics